“Beating the devil out of it”
Being the Bob Ross of
your own patient assessment
“People will forget what
you said, people will forget what you did, but people will never forget how you
made them feel.”
~Maya Angelou
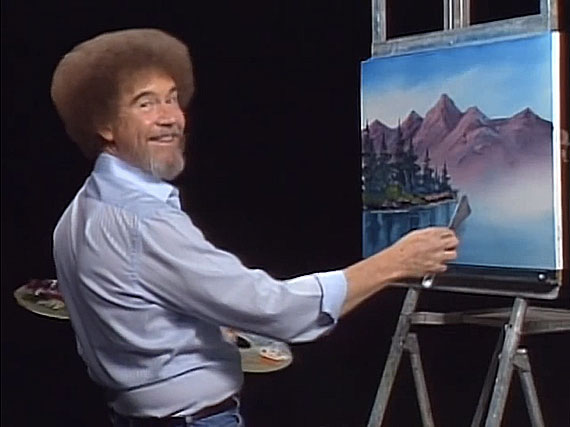
We all remember spending those
afternoon lunch hours as either kids or adults being sat down in front of the
TV to watch the patron saint of nap time, Bob Ross. Bob Ross created for
himself a great persona. He knew the basic skills of painting and he adapted
the skills to meet his personality. Bob was great as to use his own sayings to
show you what he really meant. One of those that sticks in my Mind is his
famous saying when he was cleaning a paint brush. “Beat the devil out of it”,
he would say. Not many painters might say that, but that was Bob Ross’s own
saying that he developed. When it comes to EMS we have our own art form. The
art form that I am referring to is patient assessment. Patient assessment is at
the very least an art form. Some can draw stick figures and others can paint
the Mona Lisa when it comes to assessing the sick or wounded.
Patient assessment as you hear from
your EMS educators must follow the sheet from top to bottom. The problem is
this we are teaching students to repeat phrases that they don’t understand. We
use acronyms that we hold up on a pedestal. It’s almost like when you take an
EMT class you have won the golden ticket and can now fully understand the
acronym. To be one us in EMS, you must then memorize these absurd acronyms that
may work only for pain (OPQRSTI) or you can’t remember from class like
DAGCPETER.
These holier than thou
acronyms are a struggle for a lot of students to learn, and they spend a good
part of class time studying these phrases. Instead I believe we should be
teaching them how to communicate with patients and being a good historian.
We need to be teaching students in
the field and the class room like Bob Ross did. Give them the basic tools to
succeed in communicating with their patient. But as Ross would say, “It’s your
world create it how you like it, if you want a tree place a tree there”. Too many times we tell people they must get a
set of vital signs at this point in the assessment, no sooner or later. However,
prehospital practitioners are obtaining vitals as soon as they arrive on scene.
Is this a bad practice, by no means? We need to have a change in mind set.
Another example of teaching to the book, is the way we make sure a patient is
alert and orientated. The gold standard is that they must ask 4 questions. Now
if you ask the following questions you may be right out of EMT class.
-What is your name?
-What is today?
-Where are we at?
-What is Going on
today
Now if you have been in EMS for a
while you may ask the following questions just based on your preference. You
got the basic tools in class but you have adapted questions that you know the
answers to. Maybe you have seen success with these four questions. From these questions,
you can determine if a zombie is A/O x4, or if your grandmother is out of her
mind. So, what I’m going to give you is some basic points to improving, enhancing
or maintaining your patient assessment in the prehospital field.
1.
Scene size up doesn’t stop after
arriving on scene
When we all started in class, our
teachers had us say a phrase possibly like, BSI my scene is my scene safe. The question I want to know is, do you really
know if your scene is safe or are you relying on someone else to make that
decision for you. Then when you approach
the scene and enter with this safety mindset are you continuing that throughout
the call. Are you mindful of the child crying in the back room while you’re
taking care of the sick mother in the front room. Scene size up does not have to be just guns,
knives and cocaine oh me. It could be, who is going to take care of your child
while we are gone. Possibly it could be why is there only cat food in granny’s
refrigerator. Scene size up and assessment doesn’t stop until your back at the
station.
2.
A good history today, may save a patient’s
life tomorrow
OPQRSTI only works for pain. You can adapt for other problems going on.
you can look for associated signs and symptoms with your working diagnosis.
Based on their chief complaint you can make your differential diagnosis and
work from there. You may add possibilities and subtract ones as you progress
through. All in all, remember that what they tell you is most likely what is
going on. The patient is the best caregiver. They don’t have the medical training
like we do, to take care of their issue or identify the critical nature of
their problem. With great power comes great responsibility as peter parker
said. So, if a patient tells you something you think is important in their
history than pass it along. It could be the difference of them living or not.
3.
ALWAYS, ALWAYS, ALWAYS, ask for
allergies before giving a medication
never ever assume the patient doesn’t
know what they are talking about or that most people are not allergic to this
medication. Complacency kills. Even when administering such drugs as Zofran,
Aspirin, or Benadryl ask for allergies. They are medications and people can
have bad reactions to these medications. Always be that advocate for your
patient.
4.
Remember their Name
Too many times we show up on scene
and start taking care of someone. It isn’t till we are showing up at the hospital,
the nurse asks the patients name we have a dumbfounded look upon our face because
we never asked their name. Even worse we asked their name but we forgot it. If
you are not good a remembering like I am, write it down. You will create that
much more rapport with your patient just by remembering their god given name.
So, remember as Bob ross would say, "Maybe in our world there lives a happy little tree over there," you may have a few more clouds in your patient assessment than someone else .
 Each patient assessment
is unique but everyone was given the basic concept of providing excellent
patient care. How you choose to paint your clouds or place your trees is up to
you. Just remember we are advocates of our patients and they depend on us to
provide top notch prehospital care.
Each patient assessment
is unique but everyone was given the basic concept of providing excellent
patient care. How you choose to paint your clouds or place your trees is up to
you. Just remember we are advocates of our patients and they depend on us to
provide top notch prehospital care.
Do the best you can until you know better. Then when you
know better, do better
~ Maya Angelou




Comments
Post a Comment